The midwest region has the lowest survival rate for many of Ireland’s most common cancers, according to a new report from the National Cancer Registry of Ireland (NCRI).
The midwest consistently ranked below the national average when it came to the five-year survival rate, and frequently at the bottom of the table compared to the country’s other regions.
This comes as the HSE transitions towards six new health regions: HSE Dublin and Northeast (DNNE), HSE Dublin and Midlands (DNML), HSE Dublin and South East (DNSE), HSE Mid West (MW), HSE South West (SW) and HSE West and North West (WNW).
Each region is to be responsible for providing both hospital and community care for the people in that area and will be fully established by early next year.
Over 400,000 people live in the midwest region, which geographically covers Clare, Limerick and North Tipperary.
The NCRI today published its annual report for 2020-2022, also covering statistics relating to cancer incidence and survival across the regions from 2009 to 2018.
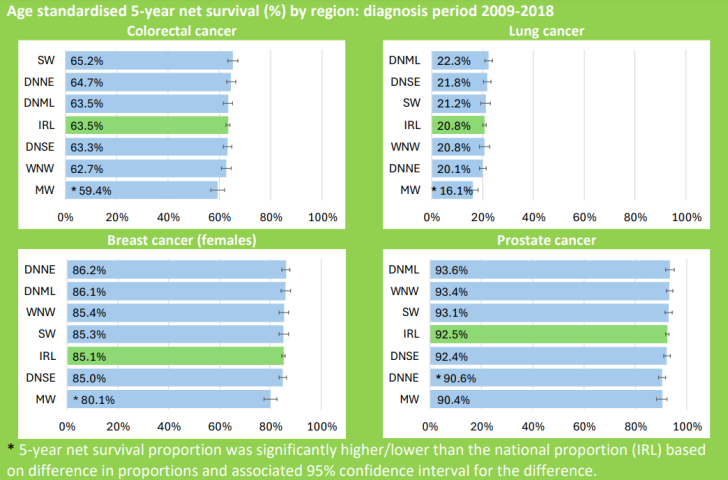
For colorectal cancer in Ireland overall, five-year net survival was 63.5 percent for cases diagnosed during 2009-2018. Five of the six health regions were found to have a similar survival rate, except for the midwest region, which had a survival rate of 59.4 per cent – 4.1 percentage points lower than the national survival proportion.
When it comes to lung cancer in Ireland overall, the five-year net survival rate was 20.8 percent for cases diagnosed during the same period. Once again, five of the six health regions showed a similar survival rate, except for the midwest region at 16.1 percent – 4.7 percentage points lower than the national survival proportion.
Female breast cancer in Ireland was a similar story, with a five-year net survival of 85.1 per cent for cases diagnosed during 2009-2018, which fell to 80.1 percent for the midwest region.
The midwest region also had the lowest survival rate (90.4 percent) for prostate cancer, but was closely followed by the Dublin and North East Area (90.6 percent).
The report stated that comparison of the five-year survival estimates across geographical regions should be interpreted with “certain caveats”, such as the fact that “late stage at diagnosis and concurrent illness will predispose to poorer survival”.
“These estimates do not adjust for stage, comorbidities, cancer case-mix and socioeconomic indicators which vary across regions,” the registry said.
Meanwhile, the impact of Covid-19 on cancer registration is also considered in the report, which found that during the first year of the pandemic (2020), “a preliminary analysis estimated that the shortfall of cancer diagnoses due to Covid-19 in 2020 was no greater than 14%”.
“After one further year of registration activity, the shortfall on projected cases for 2020 was estimated at 10% (10% for males; 10% for females) as reported in the 2022 NCRI annual statistical report,” the report reads.
For 2021, a preliminary analysis published in March 2023 showed that the estimated shortfall was
6 percent (9 percent in males; 3 percent in females), which after a further 6 months of registration activity, with registration complete, a re-calculation showed as 4 percent (7 percent for males; 1 percent for females).
“The reductions in cancer diagnoses during 2020 & 2021 are likely a result of pandemic-related
impacts on health-seeking behaviour among the public, disruptions to cancer control services and
COVID-19 related deaths among people who would otherwise have gone on to be diagnosed with
cancer,” the report states.
It was noted also that most cancers (60 percent) occur in the eastern half of the country, which is attributed to its higher population density.